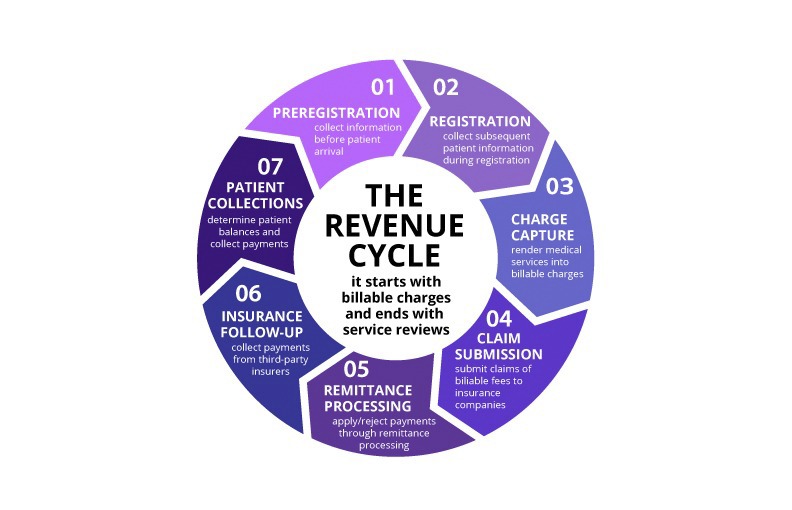
Artificial intelligence is rapidly transforming healthcare administration, offering unprecedented opportunities to improve efficiency, accuracy, and cost-effectiveness in medical billing and revenue cycle management. As AI technology becomes more sophisticated and accessible, healthcare practices of all sizes are beginning to explore how these tools can enhance their operations.
The integration of AI in healthcare administration represents more than just technological advancement – it's a fundamental shift toward data-driven decision making and automated processes that can free up human resources for higher-value activities. Understanding the current applications and future potential of AI in healthcare administration is crucial for practice leaders planning their technology investments.
Current AI Applications in Medical Billing
Today's AI applications in medical billing are already delivering measurable benefits for healthcare practices. These tools leverage machine learning algorithms to analyze patterns in billing data, identify potential issues, and automate routine tasks that traditionally required significant manual effort.
Automated coding assistance represents one of the most mature AI applications in medical billing. These systems can analyze clinical documentation and suggest appropriate procedure and diagnosis codes, helping to improve coding accuracy while reducing the time required for code assignment. Advanced systems can even identify potential compliance issues or coding inconsistencies before claims are submitted.
Claim scrubbing and error detection have been significantly enhanced by AI technology. Machine learning algorithms can identify patterns that indicate potential claim issues, such as unusual code combinations, missing information, or documentation inconsistencies. This proactive approach helps prevent denials and reduces the need for claim rework.
Predictive analytics for denial management use historical data to identify claims that are likely to be denied, allowing practices to address potential issues before submission. These systems can analyze factors such as payer patterns, code combinations, and documentation quality to predict denial risk with remarkable accuracy.
Revenue Cycle Analytics and Insights
AI-powered analytics are transforming how healthcare practices understand and optimize their revenue cycle performance. These tools can process vast amounts of data to identify trends, patterns, and opportunities that would be difficult or impossible to detect through manual analysis.
Performance benchmarking using AI can compare a practice's metrics against industry standards and peer practices, providing context for performance evaluation and identifying specific areas for improvement. These systems can account for factors such as practice size, specialty, and geographic location to provide more relevant comparisons.
Cash flow forecasting has become more accurate with AI systems that can analyze historical patterns, seasonal variations, and external factors to predict future revenue and collection patterns. This capability helps practices make more informed financial decisions and plan for potential cash flow challenges.
Payer behavior analysis uses machine learning to understand how different insurance companies process claims, identify payment patterns, and predict optimal timing for claim submission and follow-up activities. This intelligence can significantly improve collection rates and reduce payment delays.
Patient Communication and Engagement
AI is revolutionizing patient communication and engagement in healthcare administration, creating more personalized and effective interactions while reducing administrative burden on staff.
Intelligent chatbots and virtual assistants can handle routine patient inquiries about billing, insurance coverage, and payment options. These systems can provide immediate responses to common questions while escalating complex issues to human staff members. Advanced systems can even process payments and update account information.
Personalized payment plans and financial counseling use AI to analyze patient financial situations and recommend appropriate payment options. These systems can consider factors such as insurance coverage, historical payment patterns, and financial capacity to suggest payment plans that are both realistic for patients and optimal for practice cash flow.
Automated appointment reminders and follow-up communications can be customized based on patient preferences, communication history, and appointment types. AI systems can optimize timing, messaging, and communication channels to maximize patient response rates and reduce no-shows.
Fraud Detection and Compliance
AI technology is becoming increasingly important for fraud detection and compliance monitoring in healthcare administration. These systems can identify suspicious patterns and potential compliance issues that might be missed by traditional monitoring methods.
Anomaly detection algorithms can identify unusual billing patterns, such as unexpected increases in certain procedure codes, unusual patient visit patterns, or billing inconsistencies that might indicate fraud or abuse. These systems can flag potential issues for human review while maintaining detailed audit trails.
Compliance monitoring uses AI to continuously review billing practices against regulatory requirements and payer policies. These systems can identify potential compliance issues before they become problems and help practices maintain adherence to complex and changing regulations.
Documentation analysis can review clinical notes and other documentation to ensure that services are properly supported and that billing accurately reflects the care provided. This capability is particularly valuable for practices that face frequent audits or operate in high-risk specialties.
Challenges and Considerations
While AI offers significant benefits for healthcare administration, successful implementation requires careful consideration of various challenges and limitations.
Data quality and integration represent fundamental requirements for effective AI implementation. AI systems require clean, consistent, and comprehensive data to function effectively. Practices must ensure that their data collection and management processes can support AI applications and that data from different systems can be integrated effectively.
Staff training and change management are critical for successful AI adoption. Staff members need to understand how to work with AI tools effectively and how these tools fit into their daily workflows. Resistance to change can undermine even the most sophisticated AI implementations.
Cost and return on investment considerations must be carefully evaluated. While AI tools can deliver significant benefits, they also require investment in technology, training, and ongoing support. Practices need to carefully assess the potential return on investment and ensure that AI implementations align with their strategic goals.
Privacy and security concerns are particularly important in healthcare, where patient data protection is paramount. AI systems must be designed and implemented with robust security measures and must comply with all applicable privacy regulations.
The Future of AI in Healthcare Administration
The future of AI in healthcare administration promises even more sophisticated applications that will further transform how practices manage their revenue cycles and administrative operations.
Advanced natural language processing will enable AI systems to better understand and process unstructured clinical documentation, improving coding accuracy and reducing the documentation burden on providers. These systems will be able to extract relevant information from physician notes, patient communications, and other text-based sources.
Integrated workflow automation will connect AI tools across the entire revenue cycle, creating seamless automated processes that require minimal human intervention. These systems will be able to handle complex scenarios and make intelligent decisions about when to escalate issues to human staff.
Predictive modeling will become more sophisticated, enabling practices to anticipate and prevent problems before they occur. These systems will be able to predict patient payment behavior, identify potential denial risks, and recommend proactive interventions to optimize revenue cycle performance.
Real-time decision support will provide immediate guidance to staff members as they perform their daily tasks. These systems will be able to analyze current situations and provide recommendations for optimal actions, helping to ensure consistent high-quality performance across all staff members.
Preparing for AI Implementation
Healthcare practices considering AI implementation should take a strategic approach that considers their current capabilities, future goals, and available resources.
Assessment of current processes and technology infrastructure is essential before implementing AI tools. Practices need to understand their current performance levels, identify specific areas where AI could provide the greatest benefit, and ensure that their technology infrastructure can support AI applications.
Pilot programs and phased implementation can help practices learn how to use AI effectively while minimizing risk. Starting with specific applications or departments allows practices to gain experience and build confidence before expanding AI use across their operations.
Vendor evaluation should consider not only the technical capabilities of AI tools but also factors such as integration requirements, training and support services, and the vendor's experience in healthcare applications. The right vendor partnership can significantly impact the success of AI implementation.
The Human Element in AI-Enhanced Healthcare Administration
While AI can automate many routine tasks and provide valuable insights, the human element remains crucial in healthcare administration. The most successful AI implementations enhance human capabilities rather than replacing human judgment and expertise.
AI tools are most effective when they augment human decision-making rather than replacing it entirely. Staff members bring contextual knowledge, relationship skills, and judgment that AI systems cannot replicate. The goal should be to free up human resources for higher-value activities that require these uniquely human capabilities.
Continuous learning and adaptation are essential as AI technology continues to evolve. Practices that invest in ongoing education and stay current with AI developments will be best positioned to take advantage of new capabilities as they become available.
Interested in AI-Enhanced Revenue Cycle Management?
JKB Medical stays at the forefront of healthcare administration technology, including AI applications that can benefit your practice. Contact us to learn how we can help you leverage these advanced tools.
Explore AI Solutions