As we enter 2025, the medical billing landscape continues to evolve with new regulations, technology advances, and changing payer requirements. Healthcare providers must stay ahead of these changes to maintain optimal revenue cycle performance. Based on our 9+ years of experience in medical billing, here are the top five strategies that will make the biggest impact on your practice's financial health this year.
1. Implement Real-Time Eligibility Verification
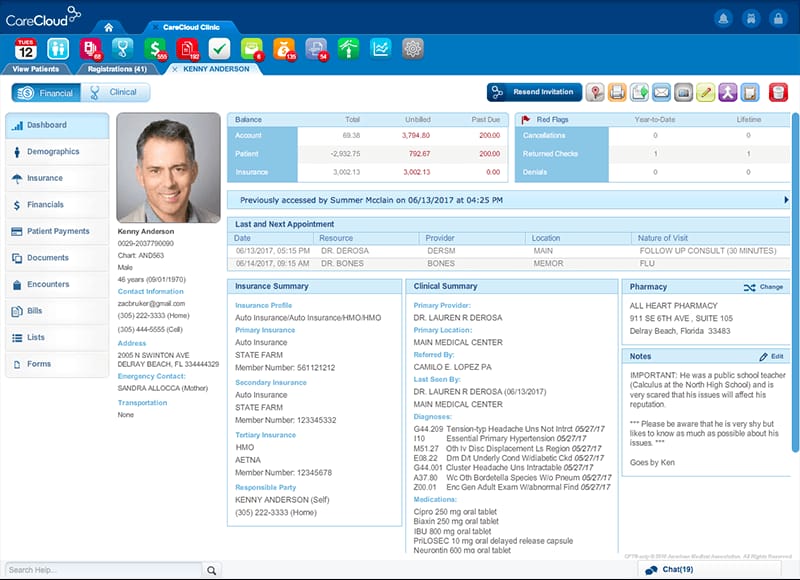
One of the most effective ways to reduce claim denials and improve cash flow is to verify patient insurance eligibility in real-time, preferably at the time of scheduling or check-in. This proactive approach can prevent many common billing issues before they occur.
Real-time eligibility verification allows you to confirm coverage details, copayment amounts, deductible information, and any prior authorization requirements. This information enables your front desk staff to collect accurate patient payments upfront and ensures that services are covered before they're provided.
Many practice management systems now offer integrated eligibility verification tools that can check coverage automatically. If your current system doesn't have this capability, consider investing in a standalone solution or upgrading your software. The cost of these tools is typically offset by the reduction in denied claims and improved collections.
2. Master Prior Authorization Management
Prior authorization requirements continue to expand across all medical specialties, making efficient authorization management crucial for maintaining revenue flow. Developing a systematic approach to prior authorizations can significantly reduce delays and denials.
Start by creating a comprehensive list of services and procedures that commonly require prior authorization from your major payers. Train your staff to identify these services during scheduling and initiate the authorization process immediately. Establish clear timelines and follow-up procedures to ensure authorizations are obtained before the service date.
Consider using authorization tracking software or creating detailed spreadsheets to monitor the status of pending authorizations. Many practices find success in designating specific staff members to handle authorizations, allowing them to develop expertise and relationships with payer representatives.
3. Optimize Your Claim Scrubbing Process
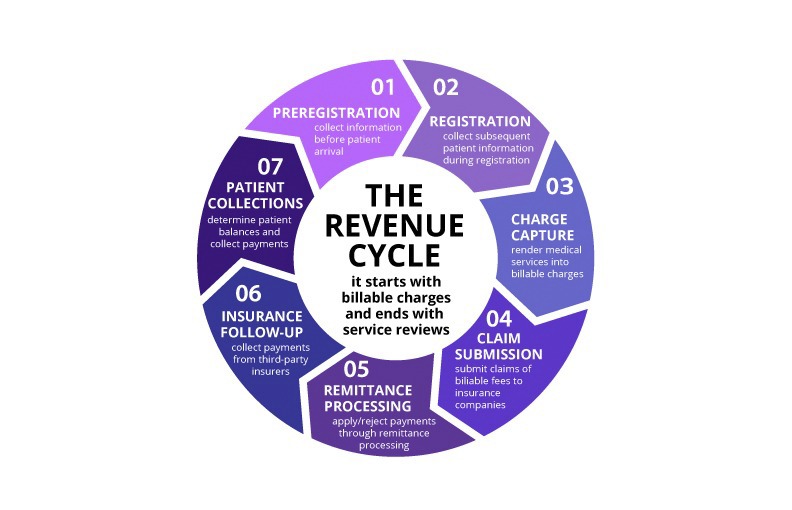
Clean claims are the foundation of efficient revenue cycle management. Implementing a thorough claim scrubbing process before submission can dramatically reduce your denial rate and accelerate payment processing.
Your claim scrubbing process should include verification of patient demographics, insurance information, procedure codes, diagnosis codes, and modifier usage. Pay special attention to common error patterns specific to your practice type. For example, DME providers should focus on documentation requirements and HCPCS coding accuracy, while optometry practices should ensure proper use of vision care versus medical eye care codes.
Many billing software solutions include built-in claim scrubbing features, but these should be supplemented with manual review processes for high-value claims or complex cases. Regular training on coding updates and payer-specific requirements is essential for maintaining scrubbing effectiveness.
4. Establish Proactive Denial Management
Rather than simply reacting to denials as they occur, successful practices in 2025 are taking a proactive approach to denial management. This involves analyzing denial patterns, identifying root causes, and implementing preventive measures.
Start by categorizing your denials into common types such as eligibility issues, coding errors, documentation problems, or authorization failures. Track denial rates by category and identify trends over time. This analysis will help you focus improvement efforts on the areas with the greatest impact.
Develop standard operating procedures for handling each type of denial, including specific timelines for appeals and rework. Train your staff on these procedures and establish clear accountability for denial resolution. Consider implementing denial prevention measures such as improved documentation templates or enhanced staff training based on your analysis.
5. Leverage Technology for Automation
Automation technology has reached a point where even small practices can benefit from implementing automated billing processes. From automated posting of electronic remittances to AI-powered coding assistance, technology can significantly improve efficiency and accuracy.
Electronic Remittance Advice (ERA) auto-posting can eliminate manual payment posting for the majority of your claims, reducing errors and freeing up staff time for more complex tasks. Many practice management systems now include this functionality, and the setup process has become much more straightforward.
Consider implementing automated patient communication tools for appointment reminders, payment notifications, and collection activities. These systems can improve patient engagement while reducing administrative burden on your staff.
For practices with higher claim volumes, explore AI-powered coding assistance tools that can help ensure accurate code selection and identify potential compliance issues before claims are submitted.
Implementing These Strategies
While these five strategies can significantly improve your billing performance, successful implementation requires careful planning and execution. Start by assessing your current processes and identifying the areas where you have the greatest opportunity for improvement.
Consider prioritizing implementations based on potential impact and available resources. For example, if you're experiencing high denial rates due to eligibility issues, real-time verification might be your first priority. If your staff is overwhelmed with manual tasks, automation might provide the most immediate relief.
Remember that change management is crucial for success. Ensure that your staff understands the benefits of new processes and provide adequate training and support during implementation. Regular monitoring and adjustment of new processes will help ensure long-term success.
The Bottom Line
The medical billing landscape in 2025 rewards practices that are proactive, technology-savvy, and focused on prevention rather than reaction. By implementing these five strategies, you can position your practice for improved financial performance and reduced administrative burden.
If implementing these strategies seems overwhelming or if you lack the internal resources to execute them effectively, consider partnering with a specialized medical billing service. Professional billing companies have the expertise, technology, and dedicated resources to implement these best practices while allowing you to focus on patient care.
Need Help Implementing These Strategies?
JKB Medical specializes in helping healthcare providers optimize their revenue cycle performance. Our team has the expertise and technology to implement these strategies effectively for your practice.
Schedule a Free Consultation